Can Fascia Be The Cause Of My Pelvic Pain?
Fascia is connective tissue, primarily made up of collagen which surrounds, attaches, and separates muscles and internal organs. You’ve probably heard of this term before as it is fast becoming a fad.
Speaking of fads, remember those days when Kinesio tape was seen on all the volleyball players’ shoulders? Then there were circular marks all over Olympic swimmers’ shoulders from cupping. These tools came to be a hot topic in the sports medicine world. It turns out that those modalities are meant to help mobilize the fascia in an effort to reduce pain and injury that could be occurring as a result of repetitive movements.
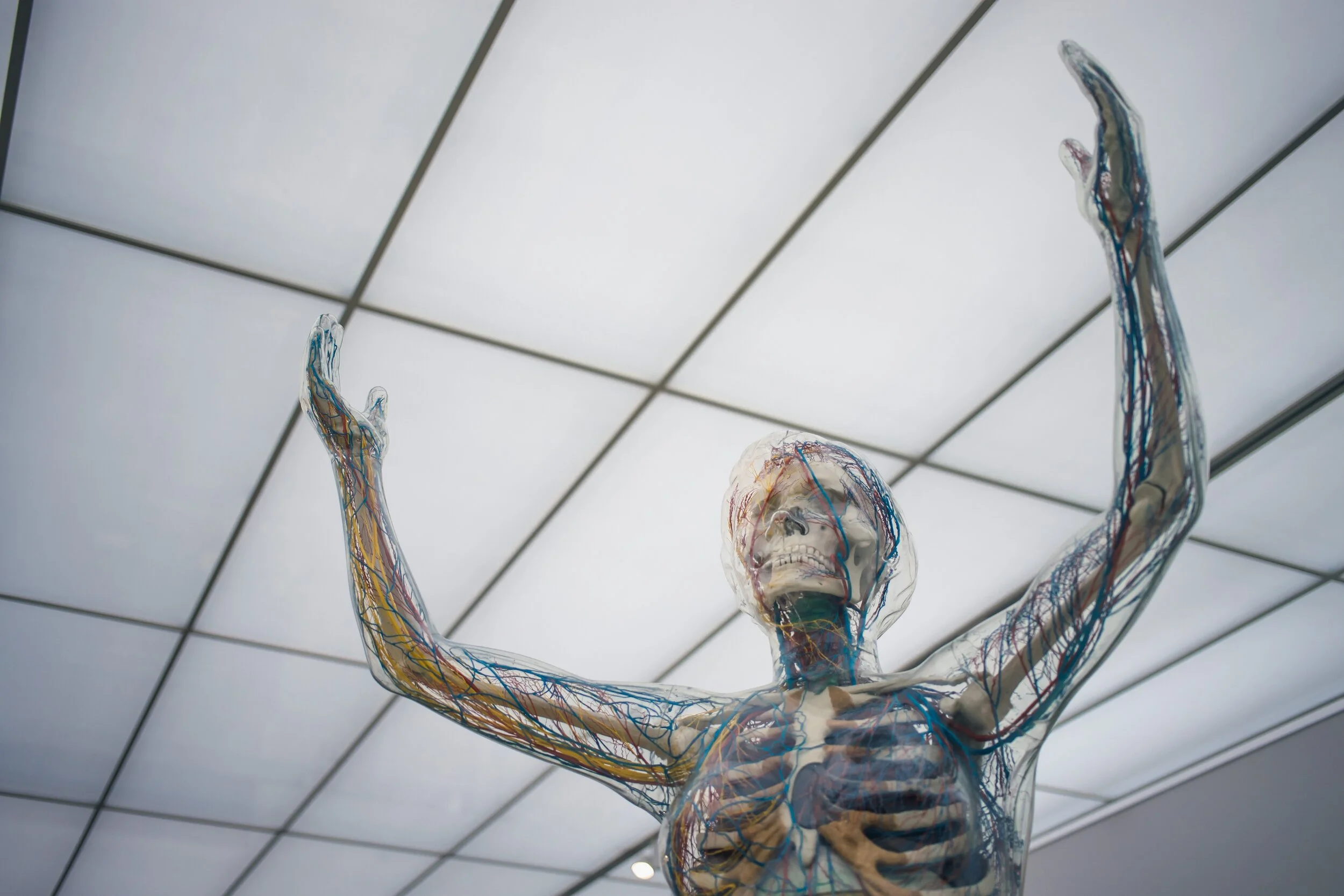
What exactly is fascia and why is it so important when it comes to pain management? There is no comprehensive definition of fascia amongst researchers, however, there is an agreement in medical texts that fascia “creates a structural continuity that gives form and function to every tissue and organ.”(1) In other words, it sort of acts like the glue that holds us together.
So, can fascia be the cause of my pelvic pain? Here is some food for thought:
1. Fascia exists in more places than you may think.
As I mentioned above, researchers have come to agree on defining fascia as a continuum throughout the body. This is important as it could explain why you might experience pelvic pain in your sacroiliac (SI) joint when a massage therapist is working on your upper glute or low back muscle. Trigger points, or small nodules more commonly known as “knots” in your muscle, can also have this effect. This is known as referred pain, which is when you feel pain somewhere else in the body other than the actual source of the pain.
For example, you might feel pain in your low back when it’s actually coming from a knot in your glute. Trigger points are important to treat as they themselves can lead to pain. I digress…my point is we need to recognize that fascia envelops, attaches, and separates not just muscle, but also tissues like nerves, organs, bones, joints, and even blood vessels. Essentially, it’s everywhere.
Let’s delve into this concept a little deeper. Have you gone to a yoga class and had trouble touching your toes while bending forward as you’re going through a vinyasa? I bet you thought to yourself, “Wow! My hamstrings must be really tight.” What if I said that maybe it’s not due to the hamstring muscles being tight, but coming from tight nerves because the fascia enveloping those nerves is bound up. Fascial tissues allow for the sliding of muscles, nerves, and vessels, organs, and other tissues. If there is some dysfunction in the fascial layer where it has built up or stiffened due to lack of movement, you can imagine how that could impact your nerves and limit the range of motion.
2. Fascia is a well-innervated structure.
Fascia contains free nerve endings and pressure receptors, making it a potential source of pain. Some of the receptors within the fascia provide us with proprioception, nociception, and interoception. Proprioception is our ability to perceive our own bodies in space. Nociception is the response of the nervous system to detect a potentially harmful stimulus. Interoception is our ability to be aware of what’s going on inside our bodies.
With these in mind, it’s clear that dysfunction in fascia plays an important role in the way we interpret and recognize pain. This could explain why you might feel so much better after a yoga class. It’s not that you have stretched a tight muscle, but actually that you have released fascial restrictions through movement in multiple planes at your end range of motion. Essentially, you have tricked your brain into perceiving pain differently by acting on the receptors that live in your fascia.
3. Consider fascia during pregnancy and postpartum.
In relation to prenatal folks, mechanical changes occurring throughout pregnancy create a prime opportunity for fascia to become more of a problem. Such changes include your center of mass shifting forward and up, strain and load increasing on muscles and joints in the low back and pelvic floor, and increased stretch to the abdominal wall. This can impact your fascial system and introduce new pain that you have never experienced before.
For the postpartum population, pelvic pain and other conditions such as diastasis recti abdominis (DRA) are common. Fascial restrictions within the abdomen can contribute to DRA and are a factor to be considered in postpartum recovery.
Research supports that movement and regular exercise helps to prevent fascial dysfunction. Other basic things like hydration, proper nutrition, and sleep contribute to healthier tissues and less inflammation throughout the body.
So if you are experiencing pain, whether it’s in the pelvis or another body part and you haven’t been able to figure out why maybe we need to look to your fascia. Give us a call to set up your free 15-minute phone consultation, today.
There are so many reasons you may hurt. We can help you understand why, and what you can do about it.
About the author:
To learn more about Dr. Anissa Akrout, PT, DPT, click here.
Citations
1. Bordoni B, Mahabadi N, Varacallo M. Anatomy, Fascia. [Updated 2019 Dec 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493232/